What is Lymphedema and Why Do I Have It: A Comprehensive Guide to Understanding Your Diagnosis
If you've recently been diagnosed with lymphedema or have noticed unexplained swelling in your arms, legs, or other parts of your body, you likely have many questions. Understanding what lymphedema is, why it developed, and how to manage it effectively can feel overwhelming at first.
This comprehensive guide will help you understand your condition and empower you to take control of your lymphedema management. Whether you're seeking lymphedema treatment in New Jersey or just learning about your diagnosis, this guide provides the essential information you need.
What is Lymphedema?
Lymphedema is a chronic condition characterized by swelling in various areas of your body, most commonly in the arms and legs. This swelling occurs when something affects your lymphatic system, preventing the normal flow and drainage of lymph fluid.
Your lymphatic system is a critical part of your immune system and circulatory network. It consists of a complex network of vessels, nodes, and ducts that work together to collect excess fluid, proteins, and toxins from your cells and tissues, returning them to your bloodstream. When this system is damaged, blocked, or unable to function properly, lymph fluid accumulates in the surrounding tissues, causing the characteristic swelling of lymphedema.

The lymphatic system: A network of vessels and nodes that helps drain fluid from tissues
Understanding Your Lymphatic System: Think of your lymphatic system as your body's drainage system. Just like a clogged drain in your sink prevents water from flowing properly, damage to your lymphatic vessels or nodes prevents lymph fluid from draining effectively, leading to a backup that causes swelling.
Why Do I Have Lymphedema? Understanding the Causes
Understanding why you developed lymphedema is an important step in managing your condition effectively. Lymphedema is generally classified into two main types based on its underlying cause: primary lymphedema and secondary lymphedema.
Primary Lymphedema: When It's Genetic
Primary lymphedema is a rare genetic condition that occurs when your lymphatic system doesn't develop properly or is missing certain components. This type affects approximately 1 in every 100,000 people in the United States. Primary lymphedema can appear at different stages of life, from infancy (congenital) through adolescence (praecox) or adulthood (tarda).
If you have primary lymphedema, it's typically caused by genetic mutations that affect the development or function of your lymphatic vessels and nodes. While this form is less common, genetic testing and early diagnosis can help guide your treatment plan.
Secondary Lymphedema: The Most Common Type
Secondary lymphedema is far more common, affecting approximately 1 in every 1,000 people in the United States. This type develops when your previously healthy lymphatic system becomes damaged or blocked. According to medical research, secondary lymphedema results from acquired lymphatic injury, obstruction, or overload.
The most common causes of secondary lymphedema include:
Cancer Treatment: This is the leading cause of secondary lymphedema in developed countries. Surgical removal of lymph nodes (lymph node dissection), radiation therapy, or tumor infiltration can all damage your lymphatic system. Breast cancer treatment is particularly associated with lymphedema risk, but other cancers affecting gynecologic, genitourinary, and head and neck areas also carry significant risk.
Surgery: Any surgical procedure that involves removing or damaging lymph nodes or vessels can lead to lymphedema. The condition may develop immediately after surgery or take months to years to appear.
Radiation Therapy: Radiation treatment can damage lymphatic vessels, making it difficult for lymph fluid to drain properly from the affected area.
Infection: Worldwide, lymphatic filariasis (a parasitic infection) remains the leading cause of lymphedema in tropical and subtropical regions. Other infections that damage the lymphatic system can also trigger lymphedema.
Trauma or Injury: Deep cuts, bruises, burns, or sports injuries that damage lymphatic vessels can result in lymphedema.
Obesity: Being significantly overweight can put extra pressure on your lymphatic system and is considered a risk factor for developing lymphedema.
Venous Insufficiency: Long-term problems with your veins can overload your lymphatic system, eventually leading to lymphedema.
Important to Know: Not everyone who undergoes cancer treatment or surgery develops lymphedema. However, understanding your risk factors can help you take preventive measures and recognize early symptoms if they occur.
Recognizing Lymphedema Symptoms
Lymphedema symptoms can develop gradually over time or appear suddenly. The severity can range from mild discomfort to significant swelling that affects your daily activities. Common symptoms include:

Common lymphedema symptoms include visible swelling, heaviness, and skin changes
Swelling in your arms, legs, hands, feet, chest, or other areas of your body
A feeling of heaviness or fullness in the affected limb or area
Restricted range of motion or tightness in your joints
Aching or discomfort in the affected area
Difficulty fitting into clothing or jewelry that previously fit well
Inability to see or feel veins and tendons in your hands and feet
Skin changes such as thickening, hardening, discoloration, or a feeling of tightness
Recurring infections (cellulitis) in the affected area
Many people first notice that one arm or leg appears slightly larger than the other, or that rings, watches, or shoes feel uncomfortably tight. You might also experience a sensation that your skin is "puffy" or notice that pressing on the area leaves an indentation.
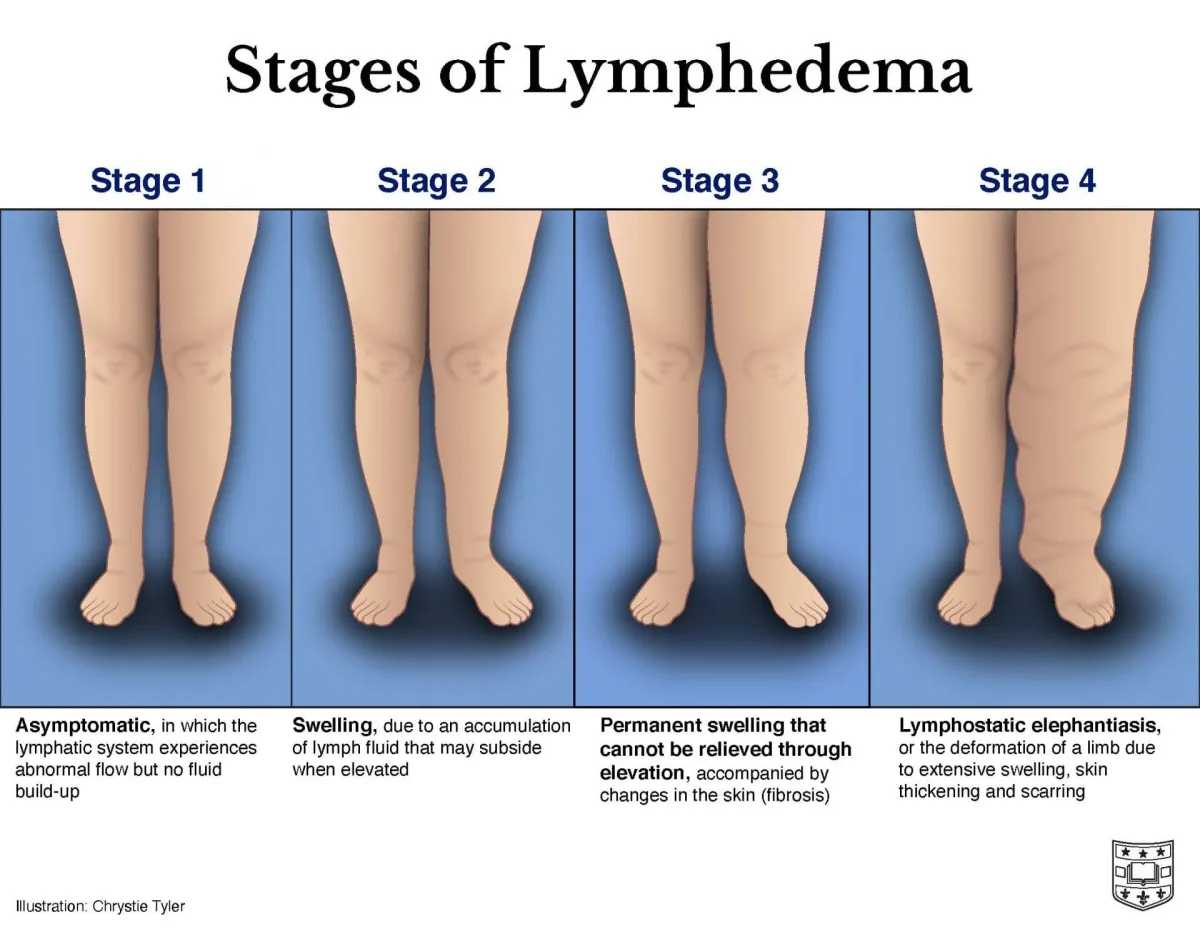
Understanding the Stages of Lymphedema
Healthcare providers classify lymphedema into different stages to help guide treatment decisions. According to Johns Hopkins Medicine, understanding which stage describes your condition is important for determining the most effective treatment approach:
Stage 0 (Latent): At this stage, there's no visible swelling yet, but you may notice subtle symptoms like a feeling of heaviness, fullness, or tightness in the area. Your lymphatic system is compromised, but swelling hasn't developed. This stage is reversible with proper intervention.
Stage 1 (Mild): Visible swelling begins to appear, and the affected area may feel heavy or full. The positive sign at this stage is that the swelling improves when you elevate the affected limb above your heart. When you press on the swollen area, it may leave a temporary indentation (called "pitting edema"). This stage is still considered reversible with treatment.
Stage 2 (Moderate): Swelling becomes more pronounced and no longer improves significantly with elevation. The tissue begins to feel firmer or spongy due to fibrosis (tissue hardening). Pressing on the area may not leave an indentation as easily. Early intervention at this stage is critical, as it may still be reversible with aggressive treatment.
Stage 3 (Severe/Lymphostatic Elephantiasis): This is the most advanced stage, characterized by significant swelling that severely limits function and movement. The skin becomes very thick, hard, and may develop a leathery appearance. Skin changes can include warty growths, deep folds, and severe fibrosis. This stage is generally not reversible, though treatment can prevent further progression and improve quality of life.
Early Detection Matters: The earlier lymphedema is diagnosed and treated, the better the outcomes. If you notice any unusual swelling or changes in how your arms, legs, or other body parts look or feel, especially after cancer treatment or surgery, contact your healthcare provider promptly.
How is Lymphedema Diagnosed?
There isn't a single definitive test for lymphedema. Instead, your healthcare provider will typically make a diagnosis based on your medical history, risk factors, and a thorough physical examination. During your evaluation, your doctor will ask about:
Your medical history, including any cancer treatments, surgeries, or injuries
When you first noticed swelling or other symptoms
Whether the swelling comes and goes or is constant
Any family history of swelling disorders
Activities or factors that make symptoms better or worse
In some cases, imaging tests may be ordered to rule out other causes of swelling or to assess the extent of lymphatic system damage. These tests might include lymphoscintigraphy (a specialized imaging study of the lymphatic system), ultrasound, MRI, or CT scans.
Treatment Options: How to Manage Your Lymphedema
While there is currently no cure for lymphedema, the condition can be effectively managed with appropriate treatment. The goal is to reduce swelling, prevent complications, maintain function, and improve your quality of life. Treatment approaches are typically individualized based on the severity of your lymphedema and your specific circumstances. Many patients in New Jersey have access to certified lymphedema therapists and specialized treatment centers throughout the state.
Compression therapy is the cornerstone of lymphedema management
Complete Decongestive Therapy (CDT)
Complete Decongestive Therapy is considered the gold standard treatment for lymphedema, especially in the early stages. This comprehensive approach is typically provided by a certified lymphedema therapist and consists of four main components:
1. Manual Lymphatic Drainage (MLD):This is a specialized, gentle massage technique that stimulates the movement of lymph fluid away from the swollen area and toward functioning lymph nodes. A trained therapist uses light, rhythmic strokes to encourage proper lymph flow.
2. Compression Therapy: After MLD reduces swelling, compression bandaging is applied to maintain the reduction and prevent fluid from accumulating again. Once swelling is controlled, you'll be fitted for compression garments (sleeves, stockings, or gloves) that you'll wear daily to prevent swelling from returning. At MCBDME, we specialize in fitting patients with the right compression garments, whether flat knit or circular knit, based on your specific needs and stage of lymphedema.
3. Exercise: Specific exercises designed by your therapist help stimulate lymphatic drainage, improve flexibility and strength, and enhance overall function. Exercise is a crucial component of long-term lymphedema management.
4. Skin Care: Meticulous skin care helps prevent infections, which can worsen lymphedema. This includes keeping skin clean and moisturized, protecting it from cuts and burns, and promptly treating any wounds or skin issues.
Compression Garments
After the initial reduction of swelling through CDT, wearing compression garments becomes a key part of your daily routine. These specially fitted sleeves, stockings, gloves, or garments help maintain the improvements achieved and prevent fluid from re-accumulating. Your lymphedema therapist will help you find the right fit and compression level for your needs.
When choosing compression garments, it's important to understand the differences between various types and brands. Our guide on how to choose compression socks compares leading brands like Medi, Juzo, and Jobst to help you make an informed decision about which compression solution works best for your lifestyle and medical needs.
Pneumatic Compression Devices
For some patients, particularly those with more advanced lymphedema, intermittent pneumatic compression (IPC) devices may be recommended. These devices use an inflatable sleeve or stocking that applies controlled pressure in specific patterns to help move lymph fluid out of the affected area. At MCBDME in Hawthorne, NJ, we provide pneumatic compression pumps that support at-home lymphedema treatment, making it easier for patients to manage their condition consistently without frequent clinic visits.
Exercise and Physical Activity
Contrary to outdated advice to avoid using affected limbs, current research supports the importance of exercise for lymphedema management. Physical activity helps stimulate lymphatic drainage, improves circulation, maintains healthy weight, and enhances overall well-being. Your healthcare team can recommend safe, appropriate exercises for your specific situation.
Weight Management
Maintaining a healthy body weight is important for lymphedema management. Excess weight can put additional strain on your lymphatic system and make symptoms worse. If you're overweight, even modest weight loss can help improve your symptoms.
Surgical Options
For severe lymphedema that hasn't responded to conservative treatments,surgical interventionmay be considered. Surgical options include:
Lymphatic bypass procedures:Surgeons connect lymphatic vessels to veins to help drain excess fluid
Vascularized lymph node transfer:Healthy lymph nodes from another part of your body are transplanted to the affected area
Liposuction:Removes excess fatty tissue that has accumulated in areas with chronic lymphedema
Debulking procedures:Removes excess skin and tissue in severe cases
Surgery is typically reserved for advanced cases and is not a cure, but rather a way to improve function and quality of life. Continued use of compression garments is still necessary after surgical procedures.
Need Help Managing Your Lymphedema in New Jersey?
At MCBDME in Hawthorne, NJ, we specialize in providing comprehensive lymphedema management solutions, including compression garments, pneumatic compression devices, and expert guidance. Our certified fitters work closely with patients throughout Northern New Jersey, including Paterson, Ridgewood, and surrounding areas. Contact us today to learn how we can support your lymphedema journey.
Living with Lymphedema: Essential Self-Care Tips
Successfully managing lymphedema requires active participation in your daily care. Here are essential strategies to help you live well with lymphedema:
Protect Your Skin
Keep your skin clean and well-moisturized to prevent cracks and infections
Protect affected areas from cuts, scratches, burns, and insect bites
Use electric razors instead of traditional razors to avoid nicks
Wear gloves when gardening or doing dishes
Apply antibacterial ointment and bandages immediately to any cuts or scrapes
Use sunscreen to prevent sunburns on affected areas
Avoid Constriction
Don't wear tight jewelry, watches, or clothing on the affected limb
Avoid having blood pressure measurements, injections, or blood draws on the affected arm if possible
Don't carry heavy bags or purses on the affected shoulder
Stay Active
Engage in regular, appropriate exercise as recommended by your healthcare team
Start slowly and gradually increase activity levels
Wear your compression garments during exercise
Listen to your body and rest if you experience increased swelling or discomfort
Elevate When Possible
Elevating the affected limb above the level of your heart when resting helps gravity assist with lymphatic drainage. This can be particularly helpful at night or when watching television.
Watch for Infections
People with lymphedema are at increased risk for skin infections, particularly cellulitis. Seek immediate medical attention if you experience:
Sudden increase in swelling
Redness, warmth, or tenderness in the affected area
Fever or chills
Flu-like symptoms
Red streaks on the skin
Maintain a Healthy Diet
While there's no specific "lymphedema diet," eating a well-balanced, nutritious diet and maintaining a healthy weight supports overall lymphatic system function. Focus on whole foods, adequate protein, fruits and vegetables, and limiting processed foods and excess sodium. For detailed guidance on the best foods for lymphedema, including a free downloadable lymphedema-friendly grocery list, visit our comprehensive nutrition guide.
When to Seek Medical Help
Contact your healthcare provider if you notice:
New or increasing swelling in any part of your body
Signs of infection (redness, warmth, fever)
Sudden worsening of symptoms
Pain that interferes with daily activities
Difficulty moving the affected limb
Skin changes such as thickening, discoloration, or open wounds
Understanding Your Prognosis
The outlook for people with lymphedema has improved significantly with modern treatment approaches. While lymphedema is a chronic condition that requires ongoing management, most people can achieve good control of their symptoms and maintain an excellent quality of life with appropriate treatment and self-care.
Early diagnosis and intervention are crucial. The earlier you begin treatment, the better your chances of preventing progression to more advanced stages. With consistent care, proper use of compression garments, regular exercise, and good skin hygiene, you can minimize the impact of lymphedema on your daily life.
The Importance of a Multidisciplinary Approach
Effective lymphedema management often involves a team of healthcare professionals working together, including:
Certified Lymphedema Therapists: Specialists trained in manual lymphatic drainage and complete decongestive therapy
Physical and Occupational Therapists: Help with exercise programs and adaptive strategies
Physicians: Oversee your overall care and manage complications
Compression Garment Specialists: Ensure proper fitting of compression garments
Nutritionists: Provide guidance on weight management and nutrition
Mental Health Professionals: Support emotional wellbeing and coping strategies
Don't hesitate to ask your primary care provider for referrals to specialists who can help you manage your lymphedema effectively. If you're in New Jersey, there are excellent lymphedema treatment centers throughout the state, including facilities in Livingston, West Long Branch, Camden, Ridgewood, Toms River, and other locations across North and Central Jersey.
Finding Support and Resources
Living with a chronic condition like lymphedema can be emotionally challenging. Connecting with others who understand what you're experiencing can provide valuable emotional support and practical advice. Consider:
Joining online or in-person lymphedema support groups
Connecting with organizations like the Lymphatic Education & Research Network
Following patient advocacy groups that provide education and resources
Participating in World Lymphedema Day activities each March 6th
Conclusion: Taking Control of Your Lymphedema
Understanding what lymphedema is and why you have it is the first step toward effective management. While receiving a lymphedema diagnosis can feel overwhelming, remember that this is a manageable condition. With proper treatment, self-care, and support, most people with lymphedema can maintain good symptom control and continue to enjoy their daily activities.
The key to successful lymphedema management is early intervention, consistent treatment, and active participation in your own care. Stay informed, work closely with your healthcare team, protect your skin, wear your compression garments as directed, stay active, and don't hesitate to seek help when you need it.
Your lymphedema journey is unique to you, and with the right knowledge and tools, you can live well with this condition. Remember that you're not alone—millions of people successfully manage lymphedema every day, and with proper care and support, you can too.
Get Expert Lymphedema Support in New Jersey
MCBDME is here to help you every step of the way. Located in Hawthorne, NJ, we serve patients throughout Northern New Jersey with compression garments, pneumatic compression devices, and expert guidance. Our team includes certified fitters who understand the unique needs of lymphedema patients. Schedule a consultation today to learn how we can support your treatment plan. Call us at (973) 553-0777 or visit us at 293 Lafayette Avenue, Suite 104, Hawthorne, NJ 07506.
Medical Disclaimer:This article is for informational purposes only and is not intended to replace professional medical advice, diagnosis, or treatment. Always consult with qualified healthcare providers regarding your lymphedema management plan.
Related Articles from MCBDME:
References:
Cleveland Clinic. (2025).Lymphedema: Symptoms, Causes & Treatment
National Center for Biotechnology Information. (2025).Lymphedema - StatPearls
Mayo Clinic. (2022).Lymphedema - Symptoms and Causes
Johns Hopkins Medicine. (2025).Treating Lymphedema
Centers for Disease Control and Prevention. (2025).Lymphedema | Cancer Survivors
American Cancer Society. Lymphedema
National Organization for Rare Disorders. (2024).Primary Lymphedema
