Complete Lymphedema Guide: Treatment Options That Work
Living with chronic swelling can be frustrating, uncomfortable, and sometimes isolating. If you've noticed persistent swelling in your arms or legs that doesn't seem to go away, you might be dealing with lymphedema, a condition that affects millions of Americans but often goes undiagnosed or undertreated for years.
At MCB DME, we've spent years helping patients across Northern New Jersey understand, manage, and live well with lymphedema. This comprehensive guide will walk you through everything you need to know about this condition, from recognizing the early warning signs to exploring treatment options that can restore your comfort and mobility.

What Is Lymphedema?
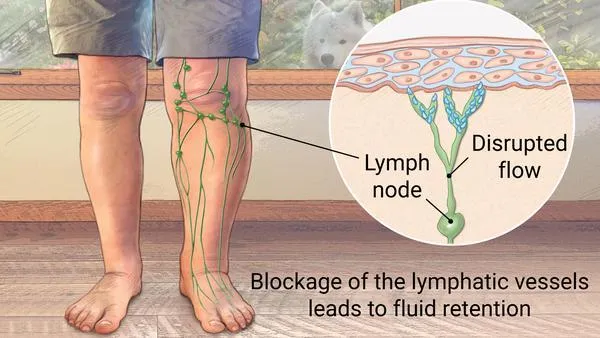
Lymphedema is a chronic condition characterized by the accumulation of lymphatic fluid in the body's tissues, most commonly affecting the arms or legs. This buildup occurs when the lymphatic system—which normally drains fluid and filters waste from your tissues—becomes damaged, blocked, or simply doesn't work properly.
Think of your lymphatic system as a drainage network throughout your body. When this network gets disrupted, fluid starts backing up, leading to swelling that can range from mild puffiness to severe, debilitating enlargement of the affected limb.
The condition affects approximately 3 to 5 million people in the United States alone, though many experts believe these numbers are significantly underreported. Women are more likely to develop lymphedema than men, particularly those who have undergone cancer treatment involving lymph node removal or radiation therapy.
Primary vs. Secondary Lymphedema: Understanding the Difference
Lymphedema is generally classified into two main categories, each with distinct causes and characteristics.
Primary lymphedema is relatively rare and stems from developmental abnormalities in the lymphatic system that are present from birth. These genetic or congenital issues may not manifest until later in life, sometimes appearing during puberty, pregnancy, or even middle age. In these cases, the lymphatic vessels are either missing, too narrow, or otherwise malformed, preventing proper fluid drainage from the start.
Secondary lymphedema is far more common and develops as a result of damage to a previously normal lymphatic system. This damage can occur from various causes including cancer treatment (surgery or radiation that affects lymph nodes), infection, trauma, or even obesity. For many patients, secondary lymphedema develops following breast cancer treatment, as surgical removal of underarm lymph nodes or radiation therapy to the chest area can significantly impair lymphatic drainage in the arm.
Understanding which type you have can help guide treatment approaches and set realistic expectations for management, though the day-to-day treatment strategies often overlap considerably.

Recognizing the Signs: Lymphedema Symptoms
Early detection of lymphedema can make a significant difference in treatment outcomes, yet many people dismiss initial symptoms as temporary swelling or simply gaining weight. Knowing what to watch for can help you seek treatment before the condition progresses.
Early-stage symptoms often begin subtly. You might notice that your arm or leg feels heavier than usual, even though visible swelling may be minimal or absent. Jewelry, watches, or shoes that previously fit comfortably may suddenly feel tight. The skin might have a slightly puffy appearance, and when you press on the area, it may leave a temporary indentation—a sign called "pitting edema."
As lymphedema progresses to moderate stages, swelling becomes more obvious and persistent. The affected limb noticeably increases in size, and the skin may start to feel tight or stretched. You might experience a reduced range of motion in the joints of the affected limb, making everyday activities more challenging. Some patients describe sensations of heaviness, achiness, or tightness that interfere with daily life.
Advanced lymphedema brings more severe complications. The skin becomes thickened and hardened, a condition known as fibrosis. The limb may develop a "woody" texture, and skin changes like discoloration, warts, or skin folds may appear. At this stage, the risk of infection increases significantly because the compromised lymphatic system can't effectively fight bacteria. The affected limb can become several times its normal size, severely limiting mobility and quality of life.
Common Causes and Risk Factors
Understanding what triggers lymphedema can help you identify your risk and take preventive measures when possible. While some causes are unavoidable, awareness allows for earlier intervention and better outcomes.
Cancer treatment remains the leading cause of secondary lymphedema in developed countries. Surgical removal of lymph nodes—common in breast cancer, melanoma, gynecological cancers, and prostate cancer treatment—disrupts the natural drainage pathways. Radiation therapy can cause scarring that blocks lymphatic vessels. Studies suggest that up to 40% of breast cancer survivors may develop some degree of arm lymphedema, though this risk varies based on the extent of treatment.
Surgery and trauma beyond cancer treatment can also damage the lymphatic system. Any surgical procedure that involves removing or disturbing lymph nodes carries some risk. Severe injuries, burns, or infections that scar lymphatic tissues can similarly impair drainage. Even scar tissue from previous surgeries can gradually restrict lymphatic flow over time.
Infections such as cellulitis or filariasis (a parasitic infection common in tropical regions) can damage lymph vessels and trigger lymphedema. Recurrent infections in the same area create a vicious cycle, as each infection causes more damage to an already compromised lymphatic system.
Obesity significantly increases lymphedema risk through multiple mechanisms. Excess fatty tissue can physically compress lymphatic vessels, while inflammation associated with obesity may impair lymphatic function. Patients who are overweight before cancer treatment face higher risks of developing lymphedema afterward.
Lack of movement or prolonged immobility can contribute to fluid accumulation. The lymphatic system relies partly on muscle contractions to move fluid through the vessels, so extended periods of inactivity—whether from bed rest, a sedentary lifestyle, or reduced mobility—can allow fluid to pool in the tissues.
Diagnosing Lymphedema: What to Expect
If you suspect you have lymphedema, early diagnosis is crucial. Your healthcare provider will typically start with a detailed medical history and physical examination, asking about any surgeries, cancer treatments, infections, or family history of swelling disorders.
During the physical exam, your doctor will measure the circumference of your limbs at multiple points to document the degree of swelling and establish a baseline for monitoring. They'll assess the skin's texture, check for signs of infection, and evaluate your range of motion. The presence of Stemmer's sign—an inability to pinch and lift the skin at the base of the second toe or finger—is a strong indicator of lymphedema.
In some cases, imaging studies may be ordered to rule out other causes of swelling or to assess the lymphatic system's structure. These might include lymphoscintigraphy (a specialized scan that tracks lymphatic flow), MRI, or ultrasound. However, lymphedema is often diagnosed clinically based on history and physical findings alone.
Comprehensive Treatment Options
While lymphedema currently has no cure, it can be effectively managed with appropriate treatment, allowing most patients to maintain excellent quality of life. The key is finding the right combination of therapies for your specific situation.

Complete Decongestive Therapy (CDT)
Complete Decongestive Therapy represents the gold standard for lymphedema treatment. This multi-faceted approach combines several techniques to reduce swelling and prevent progression. CDT typically includes manual lymphatic drainage (a specialized massage technique), compression therapy, exercise, and skin care.
The intensive phase of CDT involves daily treatment sessions with a certified lymphedema therapist who performs manual drainage and applies compression bandaging. This phase typically lasts several weeks and aims to reduce limb size as much as possible. The maintenance phase then focuses on preserving these gains through ongoing self-care and compression garment use.
Pneumatic Compression Devices
Pneumatic compression pump systems have revolutionized home-based lymphedema management, offering patients a convenient and effective way to control swelling between therapy sessions. These FDA-approved devices use inflatable sleeves or garments that rhythmically compress the affected limb, mimicking the natural pumping action of the lymphatic system.
Modern compression pumps, like those offered through MCB DME's lymphedema services, feature multiple chambers that inflate and deflate in a sequential pattern, gently moving fluid from the fingers or toes toward the trunk where it can be properly drained. Patients typically use these devices for 30-60 minutes once or twice daily, and many report significant improvements in swelling, heaviness, and comfort.
The beauty of pneumatic compression therapy is that it's usually covered by Medicare, Medicaid, and most private insurance plans when prescribed by a physician. At MCB DME, we handle all the insurance paperwork and prior authorizations, then deliver and set up the device in your home, providing thorough education on proper use. Our team stays with you during your first treatment session to ensure you're comfortable and confident using the equipment.
Compression Garments
Compression garments serve as the cornerstone of lymphedema maintenance, providing consistent pressure that prevents fluid from accumulating while allowing you to move freely throughout your day. These specially designed sleeves, gloves, socks, or stockings come in various compression levels, styles, and sizes to match your specific needs.
Proper fitting is absolutely critical for compression garments to work effectively without causing harm. Ill-fitting garments can create pressure points, restrict circulation, or simply fail to provide adequate compression. That's why professional fitting services are essential, ensuring your garment provides therapeutic compression while remaining comfortable enough to wear consistently.
Most patients need to replace compression garments every 3-6 months as they lose elasticity with regular use and washing. Many insurance plans cover multiple pairs annually, allowing you to have fresh garments on hand and ensuring you're never without compression while one set is being washed.
Exercise and Movement
Contrary to what you might expect, regular exercise is not only safe but highly beneficial for lymphedema management. Physical activity engages muscles that help pump lymphatic fluid through the vessels, preventing stagnation and reducing swelling.
The key is choosing appropriate activities and wearing proper compression during exercise. Low-impact activities like walking, swimming, yoga, and cycling are particularly beneficial. Resistance training can also be incorporated gradually, with proper guidance from your healthcare team. Many patients find that consistent exercise not only helps control swelling but also improves overall strength, energy levels, and emotional wellbeing.
Skin Care and Infection Prevention
Meticulous skin care forms an essential but often overlooked component of lymphedema management. The compromised lymphatic system makes affected limbs more vulnerable to infection, and even minor cuts, scratches, or insect bites can lead to serious cellulitis requiring hospitalization.

Daily skin care should include gentle cleansing with pH-balanced products, thorough drying (especially between fingers or toes), and application of a quality moisturizer to prevent cracking. Inspect your skin daily for any signs of injury, redness, or infection. Avoid activities that might damage the skin, such as cutting cuticles, and always wear protective gloves when gardening or doing dishes.
If you notice any signs of infection, including redness, warmth, red streaks, fever, or increased swelling, contact your healthcare provider immediately. Prompt antibiotic treatment can prevent minor infections from becoming serious complications.
Living Well With Lymphedema: Practical Tips
Managing lymphedema successfully extends beyond formal treatment sessions to encompass everyday choices and habits. Here are evidence-based strategies that can make a meaningful difference in your daily life.
Maintain a healthy weight. Excess weight places additional strain on your lymphatic system and makes swelling worse. Even modest weight loss can significantly improve lymphedema symptoms and make management easier.
Stay active within your limits. Regular movement throughout the day helps prevent fluid from pooling. If you have a desk job, set reminders to stand and move every hour. When traveling, book an aisle seat so you can easily get up and walk during flights.
Elevate when resting. Whenever possible, elevate your affected limb above heart level while resting. This uses gravity to assist lymphatic drainage, helping reduce swelling. Even 15-20 minutes of elevation several times daily can help.
Wear your compression consistently. Compression garments only work when you wear them. Make it part of your daily routine, putting them on first thing in the morning before swelling accumulates. If you struggle with donning garments, ask your provider about donning aids or consider garments with zippers for easier application.
Protect your limb from injury and temperature extremes. Avoid blood pressure measurements, needle sticks, or IV lines in the affected arm whenever possible. Be cautious with heat exposure (hot tubs, saunas, heating pads), which can increase swelling. Similarly, protect against extreme cold, which can reduce circulation.
Avoid restrictive clothing and jewelry. Tight sleeves, elastic bands, or constricting jewelry can impede lymphatic flow. Choose loose, comfortable clothing that doesn't leave marks on your skin.
Stay hydrated. Drinking adequate water supports overall lymphatic function. Despite what intuition might suggest, restricting fluids doesn't reduce lymphedema and may actually worsen it by concentrating proteins in the tissues.
The Emotional Impact of Lymphedema
Living with a chronic, visible condition takes an emotional toll that shouldn't be minimized. Many patients experience anxiety about their appearance, frustration with physical limitations, or worry about progression. Some feel self-conscious about wearing shorts or short sleeves, leading to social isolation.
These feelings are completely valid and common. Connecting with support groups—whether in-person or online like Facebook, where there are many—can provide emotional validation and practical tips from others who truly understand the challenges. Mental health support from a counselor familiar with chronic illness can also be invaluable for developing coping strategies and maintaining quality of life.
Remember that lymphedema doesn't define you. With proper management, most people with this condition continue to work, travel, exercise, and enjoy life fully. The key is finding a treatment routine that works for your lifestyle and sticking with it consistently.
Why Choosing the Right DME Provider Matters
The durable medical equipment provider you choose can significantly impact your lymphedema management success. Not all providers offer the same level of expertise, service, or support—and these differences matter when you're managing a complex, chronic condition.
At MCB DME, we specialize specifically in lymphedema and compression therapy. Our team includes certified fitters and wound care specialists who understand the nuances of lymphedema management. We don't just deliver equipment—we provide comprehensive education, ongoing support, and hands-on training to ensure you get maximum benefit from your therapy.
We handle all insurance paperwork and prior authorizations, so you can focus on your health rather than bureaucratic hassles. Our spotless facility in Hawthorne, New Jersey provides comfortable, professional fitting services, and we offer delivery throughout Northern New Jersey. When you work with us, you're not just getting equipment—you're getting a partner committed to your long-term success.
Taking the Next Step
If you're experiencing persistent swelling or have been diagnosed with lymphedema, don't wait to seek help. Early intervention can prevent progression and preserve your quality of life. Talk to your physician about whether compression therapy might be right for you—most patients are surprised to learn that these highly effective treatments are covered by insurance and available with a simple prescription.
Whether you need a pneumatic compression pump, custom-fitted compression garments, or simply guidance on managing your condition, our team is here to help. Contact MCB DME at (973) 553-0777 or visit us at 293 Lafayette Avenue, Suite 104, in Hawthorne, NJ to learn more about how we can support your lymphedema management journey.
Remember: lymphedema is manageable, and with the right treatment plan and support system, you can live a full, active, comfortable life. You don't have to face this condition alone.
